Effects of Anesthesia on the Blood-Brain Barrier
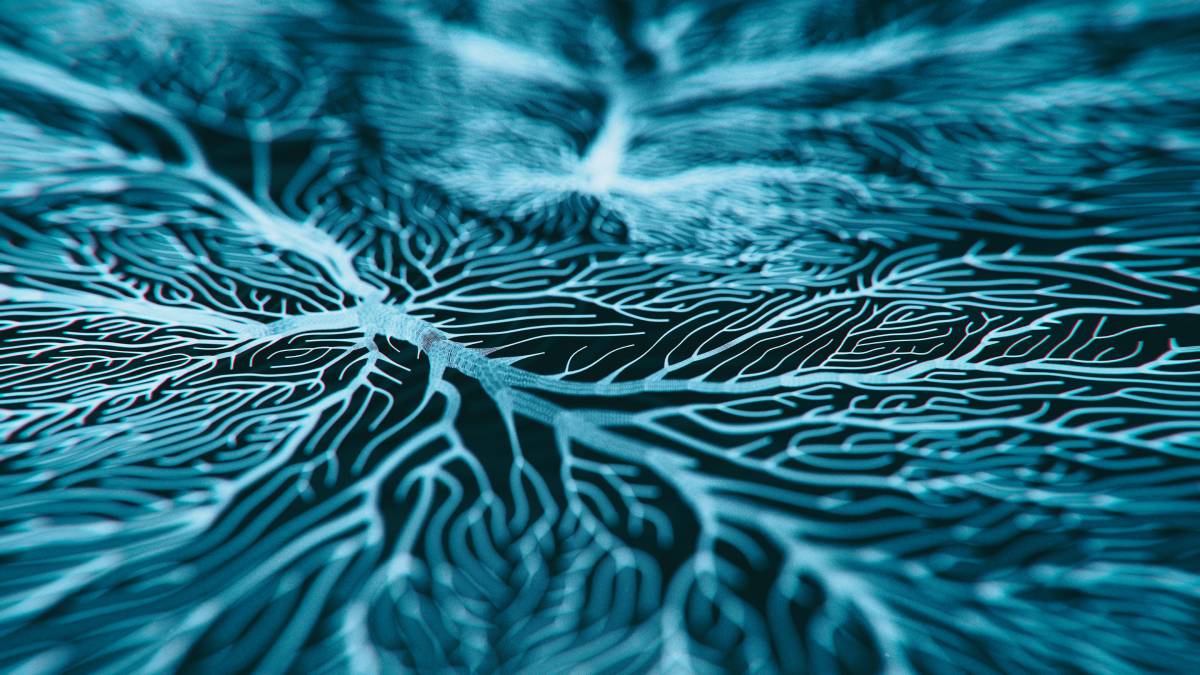
The blood-brain barrier (BBB) separates the central nervous system (CNS) from peripheral blood circulation.1 Both blood vessel and endothelial cells form the BBB; specifically, endothelial cells line the microvasculature in the CNS.2,3 The BBB limits pathogen and toxin entry to the brain’s microenvironment in order to maintain homeostasis for the CNS.1,4,5 This safe environment helps optimize normal neuronal function.4 Certain types of anesthesia may affect the characteristics of the blood-brain barrier; further research is needed to clarify this relationship.
In the BBB, tight junctions made up of claudin and occludin proteins control the movement of substrates into the CNS .3 These tight junctions connect adjacent endothelial cells by their lateral membranes. Nanometer-scale pores constrain paracellular transport between endothelial cells while allowing the transport of certain small molecules. Efflux pumps and solute carrier transporters in endothelial cells mediate transcellular molecular passage. Critically, tight junction dysregulation potentially contributes to a loss of BBB integrity and BBB breakdown.4
The BBB regulates the movement of peptides, nutrients such as glucose, and waste products into and out of the CNS. Importantly, it also regulates the transport of medications.3 Passive and active mechanisms contribute to the BBB’s highly selective nature.6 Passive diffusion across the lipid bilayer allows small, lipophilic molecules across the membrane. P-gp transporters, on the other hand, actively transport specific molecules.
A compromised blood-brain barrier may contribute to cognitive impairment, brain damage, and neurodegenerative disorders.1 An intact BBB protects the fluid and substrate homeostasis of the brain, preventing edema.7 In particular, CNS function declines in the presence of inflammation, which may originate from outside the BBB.8 In animal models, BBB disruption also plays a role in cognitive impairment in Alzheimer’s disease, cerebral ischemia, hypertension, and type 2 diabetes mellitus.1 In addition, research links increased BBB permeability to proinflammatory cytokine transport and β-amyloid clearance.1 Weakened BBB integrity may also be related to the cognitive decline that accompanies healthy aging.9
Similarly, research indicates that anesthesia potentially alters cognitive function as well. For example, anesthesia likely contributes to postoperative cognitive impairment in rodents, potentially via increased neuroinflammation, Aβ accumulation, and dysregulated mitochondrial homeostasis.10-12
Research also suggests that different anesthetics – particularly volatile ones – modulate BBB permeability.2,5,7 Yang et al., for example, hypothesized that anesthesia specifically induces age-dependent blood-brain barrier dysfunction in mice.2 Volatile anesthetics may disrupt BBB integrity via vasodilation, though other studies suggest alternate pathways, such as isoflurane-induced apoptosis and altered tight junction structure.5,13
Consequently, blood-brain barrier disruption may explain the mechanism by which anesthesia contributes to postoperative cognitive impairment. Interestingly, however, one study found the anesthesia-induced damage to the BBB to be reversible, yet the cognitive decline still persisted even after BBB recovery.5 Much of the present research uses in vitro models and rodents to study this phenomenon. Thal et al., however, posits that healthy brain tissue potentially compensates for the changes that volatile anesthetics indue.7 These models – and rodents – may detect BBB dysfunction even as it overestimates the effect in healthy brain tissue. As anesthesia is a critical part of surgery, more research needs to further clarify the relationship between anesthesia, the blood-brain barrier, and cognitive impairment.
References
1. Zlokovic, B. V. The blood-brain barrier in health and chronic neurodegenerative disorders. Neuron 57, 178–201 (2008). https://doi.org/10.1016/j.neuron.2008.01.003.
2. Yang, S. et al. Anesthesia and Surgery Impair Blood–Brain Barrier and Cognitive Function in Mice. Front. Immunol. 8, (2017). https://doi.org/10.3389/fimmu.2017.00902.
3. Viscusi, E. R. & Viscusi, A. R. Blood–brain barrier: mechanisms governing permeability and interaction with peripherally acting μ-opioid receptor antagonists. Reg. Anesth. Pain Med. 45, 688–695 (2020). https://doi.org/10.1136/rapm-2020-101403.
4. Hu, N. et al. Involvement of the blood–brain barrier opening in cognitive decline in aged rats following orthopedic surgery and high concentration of sevoflurane inhalation. Brain Res. 1551, 13–24 (2014). https://10.1016/j.brainres.2014.01.015.
5. Cao, Y. et al. Isoflurane anesthesia results in reversible ultrastructure and occludin tight junction protein expression changes in hippocampal blood–brain barrier in aged rats. Neurosci. Lett. 587, 51–56 (2015). https://doi.org/10.1016/j.neulet.2014.12.018.
6. Theodorakis, P. E., Müller, E. A., Craster, R. V. & Matar, O. K. Physical insights into the blood-brain barrier translocation mechanisms. Phys. Biol. 14, 041001 (2017). https://doi.org/10.1088/1478-3975/aa708a.
7. Thal, S. C. et al. Volatile Anesthetics Influence Blood-Brain Barrier Integrity by Modulation of Tight Junction Protein Expression in Traumatic Brain Injury. PLoS ONE 7, (2012). https://doi.org/10.1371/journal.pone.0050752.
8. Girard, T. D. et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit. Care Med. 38, 1513–1520 (2010). https://doi.org/10.1097/CCM.0b013e3181e47be1.
9. Kanner, A. A. et al. Serum S100β: A noninvasive marker of blood-brain barrier function and brain lesions. Cancer 97, 2806–2813 (2003). https://doi.org/10.1002/cncr.11409.
10. Wan, Y. et al. Postoperative impairment of cognitive function in rats: a possible role for cytokine-mediated inflammation in the hippocampus. Anesthesiology 106, 436–443 (2007). https://doi.org/10.1097/00000542-200703000-00007.
11. Wan, Y. et al. Cognitive decline following major surgery is associated with gliosis, β-amyloid accumulation, and τ phosphorylation in old mice. Crit. Care Med. 38, 2190–2198 (2010). https://doi.org/10.1097/CCM.0b013e3181f17bcb.
12. Li, Z.-Q. et al. Activation of the canonical nuclear factor-κB pathway is involved in isoflurane-induced hippocampal interleukin-1β elevation and the resultant cognitive deficits in aged rats. Biochem. Biophys. Res. Commun. 438, 628–634 (2013). https://doi.org/10.1016/j.bbrc.2013.08.003.
13. Iida, H., Ohata, H., Iida, M., Watanabe, Y. & Dohi, S. Isoflurane and sevoflurane induce vasodilation of cerebral vessels via ATP-sensitive K+ channel activation. Anesthesiology 89, 954–960 (1998). https://doi.org/10.1097/00000542-199810000-00020.