Enhanced recovery after surgery (ERAS) programs aim to expedite patients’ recovery and reduce their morbidity following surgical procedures [1]. These protocols have led to demonstrably fewer complications and shortened hospitalization stays in the United States and Europe [2]. ERAS has challenged the perception of medical teams as specialized and separate silos by encouraging hospitals to follow a more collaborative framework across all levels of professionals [3]. An essential component of enhanced recovery programs is the use of multimodal analgesia, which can involve turning to regional anesthesia [1].
A primary goal of ERAS anesthesia protocols is greater anesthesiologist involvement throughout a patient’s hospital stay [3]. Currently, the norm is that anesthesia providers are largely limited to interacting with patients only during surgery [3]. Once the surgery is over, the anesthesia provider will often move on to the next patient [3]. ERAS strives to break this norm by giving anesthesia teams the time and encouragement to check in with patients following surgery [3]. By interacting with patients more, anesthesiologists can learn about the efficacy of their treatments, especially over the long term [3]. Regional anesthesia often requires a team approach, supporting its suitability in ERAS contexts [4].
Beyond patient interactions, enhanced recovery programs also prescribe changes to fluid protocol and pharmacologic administration [3]. Contrary to the long-held belief that patients should fast the night before surgery, ERAS dictates that patients should drink carbohydrates two hours before receiving anesthesia [3]. Medical teams should also minimize opioid use, avoid long-acting preoperative sedatives, and administer short-acting anesthetics instead of longer-acting ones [3]. Collectively, these changes may encourage patients to eat and drink sooner after surgery and reduce nausea [3].
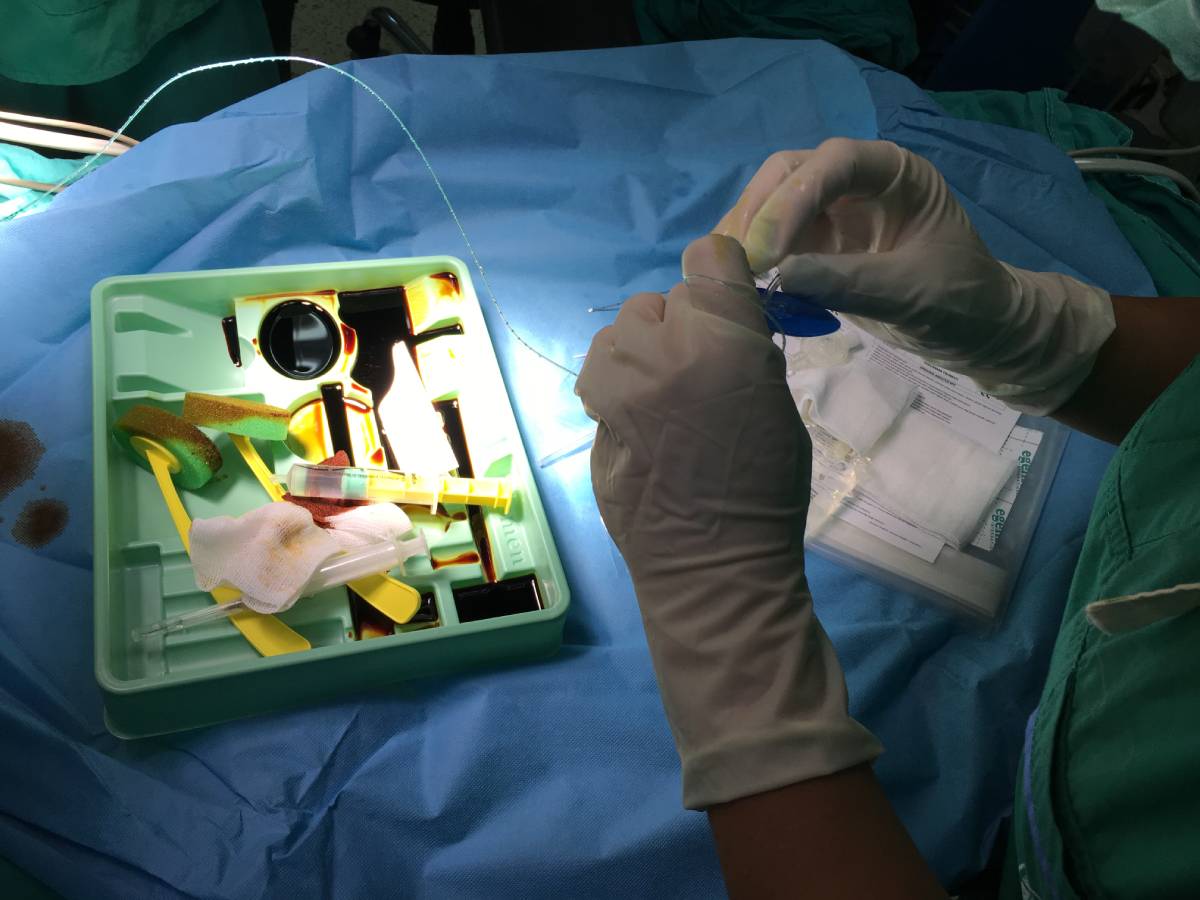
Surgeons created ERAS to improve patient outcomes following colorectal surgery, but now, medical institutions apply the program in other surgical contexts as well [3]. Still, due to its origins, most of the research conducted about ERAS programs relates to colorectal procedures. Helander et al. conducted a study analyzing fifteen institutions following ERAS protocols in New Zealand to determined which types of regional anesthesia techniques are most commonly used in the context of colorectal surgeries [1]. Thoracic epidural analgesia (TEA) came first, followed by transversus abdominis plane (TAP) block [1]. ERAS programs commonly advocate for TEA, due to its associations with improved intestinal blood flow, reduced opioid use, lower surgical stress, diminished risk of paralytic ileus, and improved analgesia [1]. The anesthesiologists studied used TAP blocks during laparoscopic procedures [1]. Anesthesia teams treating colorectal surgery patients should consider these anesthetic approaches when working under ERAS protocols. Still, physicians should remember that no concrete evidence exists yet to suggest that any anesthetic techniques are strictly preferable, so caution is advised [2].
Many research studies have demonstrated the positive impact of ERAS protocols on patient outcomes and experiences [1]. One such analysis, conducted by Grant et al., attempted to quantify process measure compliance for anesthesia protocols [5]. While the overall compliance rate was low, increased compliance by anesthesiologists to a formal anesthesia protocol reduced the length of hospital stays [2, 5]. A study of postoperative opioid use found that ERAS interventions led to hospitals using more opioid-free and multimodal forms of anesthesia during colorectal surgery [6]. However, postoperative opioid prescription rates did not decrease, indicating that protocols may need to be improved further [6]. To meaningfully combat the opioid epidemic, protocols could instruct clinicians to study patient histories, past opioid use, and in-hospital pain scores when prescribing postoperative pain medication [6].
Nevertheless, the number of studies on the efficacy of anesthesia-related components of ERAS protocols remains low [2]. To improve ERAS scholarship and promote better patient outcomes, medical institutions should invest in leadership, educational programs, and innovation [2]. By doing so, anesthesiologists and their peers may administer better quality healthcare to each of their patients.
References
[1] E. M. Helander et al., “Use of Regional Anesthesia Techniques: Analysis of Institutional Enhanced Recovery After Surgery Protocols for Colorectal Surgery,” Journal of Laparoendoscopic & Advanced Surgical Techniques, vol. 27, no. 9, p. 898-902, July 2017. [Online]. Available: https://doi.org/10.1089/lap.2017.0339.
[2] G. P. Joshi and H. Kehlet, “Enhanced Recovery Pathways: Looking Into the Future,” Anesthesia & Analgesia, vol. 128, no. 1, p. 5-7, January 2019. [Online]. Available: https://doi.org/10.1213/ANE.0000000000003746.
[3] O. Ljungqvist, “ERAS–Enhanced Recovery After Surgery,” Journal of Parenteral and Enteral Nutrition, vol. 38, no. 5, p. 559-566, February 2014. [Online]. Available: https://doi.org/10.1177/0148607114523451.
[4] F. Carli and A. Clemente, “Regional anesthesia and enhanced recovery after surgery,” Minerva Anestesiologica, vol. 80, no. 11, p. 1228-1233, February 2014. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/24492666/.
[5] M. C. Grant et al., “The Impact of Anesthesia-Influenced Process Measure Compliance on Length of Stay: Results From an Enhanced Recovery After Surgery for Colorectal Surgery Cohort,” Anesthesia & Analgesia, vol. 128, no. 1, p. 68-74, January 2019. [Online]. Available: https://doi.org/10.1213/ANE.0000000000003458.
[6] D. Brandal et al., “Impact of Enhanced Recovery After Surgery and Opioid-Free Anesthesia on Opioid Prescriptions at Discharge From the Hospital: A Historical-Prospective Study,” Anesthesia & Analgesia, vol. 125, no. 5, p. 1784-1792, November 2017. [Online]. Available: https://doi.org/10.1213/ANE.0000000000002510.